A Managed Care Organization Does Which of the Following
Managed care organizations are essential for providers to understand as their policies can dictate many aspects of. It is a health plan or health company which works to provide quality medical care at a cost-effective price.

Accountable Care Organizations Visual Ly Accountable Care Organization Healthcare Infographics Care Organization
Managed care health insurance that contracts with specific healthcare providers in order to reduce the cost of services to patients has a long history in the United States in.

. Managed care plans are a type of health insurance. View Chapter 9 quiz from HLSC 430 at University of Missouri Kansas City. She has assembled the following relevant information.
Federal Managed Care regulations at 42 CFR 438 recognize four types of managed care entities. Need a Personal Loan. Managed care organizations receive summaries of a patients medical file as part of the treatment planning and payment process.
Plans are paid a capitation ratethat is a fixed dollar amount per. Accreditation of managed care organizations. The reconciliation to account for overpayments or underpayments Selected.
Managed care is obligated to provide all of the mentioned services to its patients. Insurance the MCO acts as the insurance company collecting premiums. The term managed care is used to describe a type of health care focused on helping to reduce costs while keeping quality of care high.
1 1 Question 9 Which of the following payment issues should be covered in a managed care contract. Types of Managed Care Organizations MCOs Health Maintenance Organizations HMOs Preferred Provider Organizations PPOs Exclusive Provider Organizations EPOs Point-of-Service Plans POS. In addition MCOs represent organized care systems that often focus their efforts on defined populations and are accountable for desired outcomes.
Comprehensive risk-based managed care. She received12000 of dividend income. Most managed care systems utilize an HMO EPO PPO or POS network design limiting to varying degrees the number of providers from which a patient can choose whether the patient has to use a primary care physician and whether out-of-network care is.
These managed health plans may be offered through insurers or to the self-insured although they are much more common in self-insured group health plans. The payment responsibilities for uncovered services c. We review their content and use your feedback to keep the quality high.
These are designed to manage. A managed care organization by definition is an organization that practices managed care principles. How much of your care the plan will pay for depends on the networks rules.
A managed care organization is a single organization which manages the financing insurance delivery and payment to provide health care services. The Health Maintenance Organization Act of 1973 an amendment of the Public Health Service Act of 1944 established the foundation for managed care organizations and their comprehensive cost-saving methods. In such arrangements states contract with managed care organizations MCOs to cover all or most Medicaid-covered services for their Medicaid enrollees.
These providers make up the plans network. It has become the predominant system of delivering and receiving American health care since its implementation. A medical delivery system that attempts to manage the quality and cost of medical services that individuals receive.
Kaiser Permanente KP is a managed care organization known for its excellence and integrated care for over 9 million members Strandberg-Larsen et al 2010. Comprehensive risk-based managed care primary care case management PCCM and limited-benefit plans. Who are the experts.
This creates a lack of privacy in regards to individual medical issues or concerns that take place. Cities began providing prepaid. Plans which reimburse providers for individual health care services rendered managed care is financed.
Medicaid managed care provides for the delivery of Medicaid health benefits and additional services through contracted arrangements between state Medicaid agencies and managed care organizations MCOs that accept a set per member per month capitation payment for these. The most common health plans available today often include features of managed care. The payment responsibilities for copayments b.
The term managed care or managed healthcare is used in the United States to describe a group of activities intended to reduce the cost of providing health care and providing American health insurance while improving the quality of that care managed care techniques. As an investor you can profit from the efforts that insurers take to make their managed care organizations as financially efficient and lucrative as possible. Primary care case managers contract with the state to furnish case management location coordination and monitoring services.
Healthcare organizations include providers such as hospitals doctors and other medical professionals and facilities who work together. Is responsible for the health of a group of enrollees and can be a health plan hospital physician group or health system. Managed care is specific to health care in the United States.
Within these categories however there is wide variation across states Table 1. Issues of Concern. Of its 37 hospitals 27 were named as Top Performers by TJC ie 73 of its medical centers The Joint Commission 2013.
Question 1 1 out of 1 points A managed care organization functions like Answer Correct Answer. She received 82000 in salary. Experts are tested by Chegg as specialists in their subject area.
They have contracts with health care providers and medical facilities to provide care for members at reduced costs. MCOs usually contract with a limited number of health. The origins of managed care in the United States can be traced to the late 19th century when a small number of physicians in several US.
There is a loss of privacy. Managed Care is a health care delivery system organized to manage cost utilization and quality. Generally paid fee-for-service for medical services rendered plus a monthly case management fee.
These include provider networks provider oversight prescription drug tiers and more. Which of the following are obligations of a managed care organization to its patients. A managed care organization MCO is a business group that manages the delivery of health care services through managed health care plans.
Managed Care and HMOs. State Medicaid programs use three main types of managed care arrangements. Managed care also called managed health care type of health insurance and system of delivering health care services that is intended to minimize costs.
Plans that restrict your choices usually cost you. Financing the MCO and employer negotiates a fixed premium per enrollee and the health services provided in the contract. Managed care organizations MCOs are rapidly becoming a major source of health care for the beneficiaries of both employer-funded care and of the publicly funded programs Medicaid and Medicare.
All of the above This answer is correct. Terms in this set 39 Why has there been a rise of Managed Care Organizations MCO. The principal difference between managed care and conventional health insurance payment methods is that the responsible entity ie the managed care organization MCO usually pays for and provides services either directly or through contracts with third party providers whereas conventional health insurers underwrite the cost of coverage.
State Medicaid programs use three main types of managed care delivery systems.
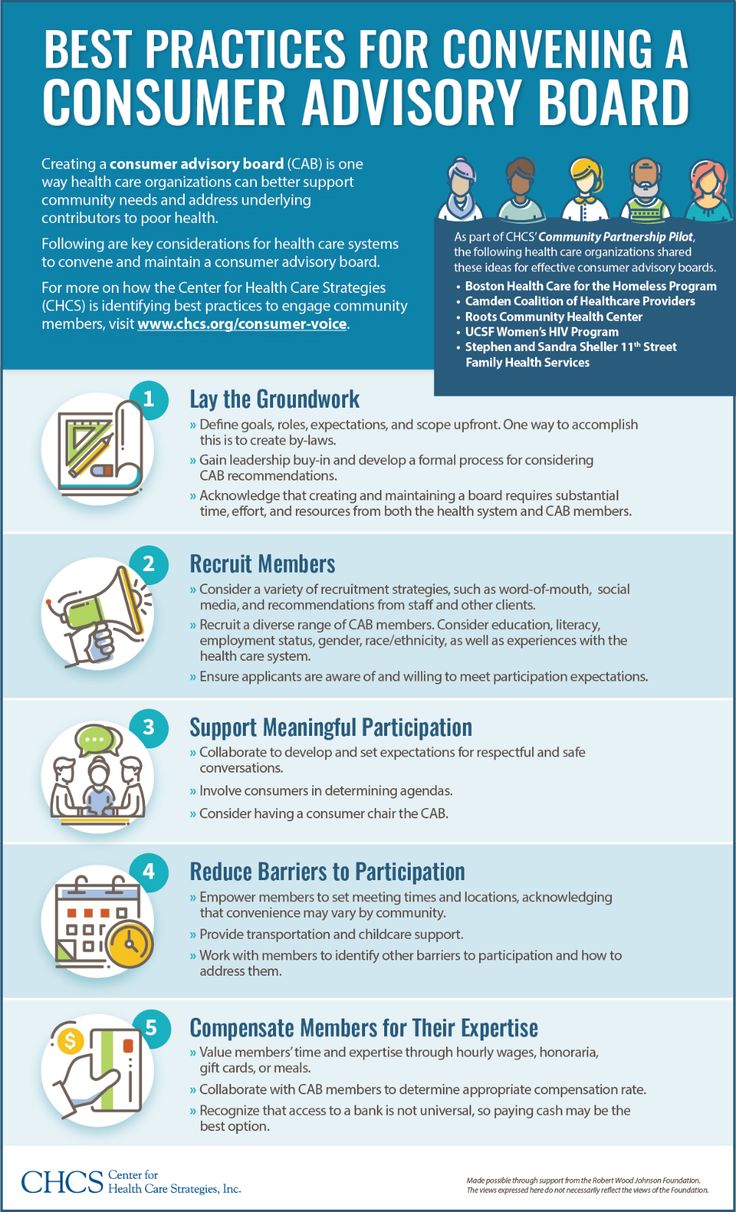
Best Practices For Convening A Community Advisory Board Healthcare System Community Engagement Care Organization

Tips For Better Use Of Managed It Services Managed It Services Business Management Network Monitor

Precision Advisors Digital Trends Study Less Than Half Of Managed Care Organizations Have Access To Electro Care Organization Health Technology Digital Trends

Project Management Fundamentals Evolving Organizations In A Competitive Business Environment Project Management Templates Project Management Project Management Tools
No comments for "A Managed Care Organization Does Which of the Following"
Post a Comment